Abstract
Background: Sickle Cell Disease (SCD) is a chronic blood disorder in which complications result from vaso-occlusion. Pain is the most common symptom reported in patients with SCD and includes both acute unpredictable pain as well as chronic pain. Chronic pain is clinically defined as having more days with pain than without pain over a period of 6 months. Various classifications systems have been developed to better understand pain phenotypes, however, there is variability in data and groupings of patients. Recent work based on patient-reported outcome data has shown that patients may be classified into three subgroups: infrequent acute pain, limited recent pain with moderate long-term pain, and persistent severe pain.
An improved understanding of the ways in which pain dynamics manifest over time will allow patients and medical providers to better manage pain. Using previously-published data which collected self-reported data through a mobile app over 6 months (Clifton et al., 2017, J. Comput. Biol.), we aimed to characterize the different ways in which patients experienced pain over time. In this work, we sought to identify classes of patients based only on their self reported pain levels.
Methods: Patients within the previously-published study were asked to self-report their pain levels from 0-10 on a daily basis through a mobile app. The study included 39 patients (16 male, 23 female), with a mean age of 33.4. Patients reported their pain an average of 0.4 times per day over an average of 164.6 days.
To allow for the possibility that patients' experiences change over time, we windowed the time series of pain dynamics into non-overlapping two-week windows. Within each window, the data were linearly interpolated to regularly-spaced samples. Then, we applied spectral clustering to identify classes of similar pain trajectories within the windowed data.
Within the data, we also identified patients with and without chronic pain within the sample based on whether or not they have taken long-acting opioid medications, which are commonly prescribed for those with a diagnosis of chronic pain. With this identification, we compared patients within the identified classes with patients diagnosed with chronic pain.
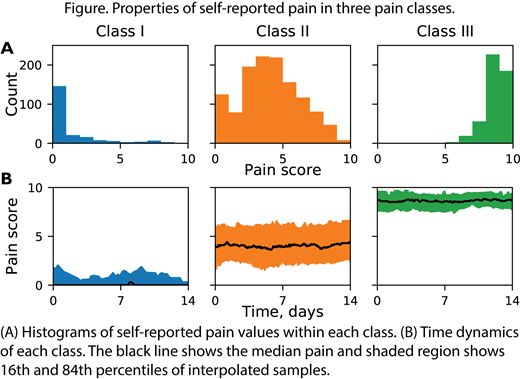
Results: We found that three classes of pain dynamics may be identified from the data considered: class I, class II, and class III (Figure). Class I pain trajectories have mild baseline pain, typically 0, with acute exacerbations of low to medium pain levels. Class II trajectories show moderate mean pain values, and show large variation within each trajectory. Class III trajectories show consistently high pain levels, rarely dropping below 7.
All three classes include patients who have been diagnosed with chronic pain, but the proportion of patients with chronic pain differs. Patients with chronic pain represented 32% of samples in class I, 83% of samples in class II, and 86% of samples in class III.
Conclusions: Based only on self-reported pain over time, clustering pain experiences into classes yields three distinct classes. These classes do not perfectly align with chronic pain diagnoses, but classes II and III both contain mostly chronic pain patients. Based on this and the unique behaviors of those classes, it may be useful to differentiate chronic pain into persistent chronic pain and intermittent chronic pain. Moreover, the findings of these classes are similar to results found from analyzing patient reported outcomes and show promise for the continued use of mHealth apps to acquire patient reported symptoms.
Shah: CSL Behring: Consultancy; Emmaus: Consultancy; Novartis: Research Funding, Speakers Bureau; Bluebird Bio: Consultancy; Guidepoint Global: Consultancy; GLG: Consultancy; Alexion: Speakers Bureau; GBT: Consultancy, Research Funding, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal